BGI Genomics 2023 Global State of Cervical Cancer Awareness Report
2023-07-20
Cervical cancer is the fourth most common cancer among women globally, with an estimated 604,000 new cases and 342,000 deaths worldwide. Few diseases reflect global inequities as much as cancer of the cervix. Nearly 90% of the deaths in 2020 occurred in low- and middle-income countries, which lag in vaccination, screening, and treatment.
In August 2020, the World Health Assembly adopted the Global Strategy for cervical cancer elimination. The WHO has set up global 90-70-90 targets to be reached by 2030: 90% of girls fully vaccinated with the human papillomavirus (HPV) vaccine by age 15; 70% of women are screened by 35, and again by 45 years of age; and 90% of women identified with cervical disease receive treatment.
To support these targets, BGI Genomics has launched a global cervical cancer awareness report to assess the level of knowledge, attitudes, and practices related to cervical cancer screening and the HPV vaccine. By examining these key areas, this survey seeks to highlight the associated barriers and opportunities.
This survey covers 1,878 women from Brazil, the Chinese mainland, Saudi Arabia, Serbia, Thailand, and Uruguay. The findings highlighted the urgent need to address barriers, improve awareness, and enhance access to screening as well as vaccination services:
HPV awareness affects cervical cancer screening rates: 40.0% of women worldwide did not know that over 95 percent of cervical cancer is caused by HPV. Among women who are unaware cervical cancer is often caused by HPV, 39.1% of them never undertaken cervical cancer screening which is higher than the global average of 31.2%.
More choice, fewer barriers: Age-specific HPV prevalence was highest in young women (<25 years) at 22%. Yet, 43.5% of women aged 21 to 25 years old - highest among the age groups surveyed - are deterred by meeting a male doctor performing a pap smear. Therefore, women, especially young women, should be offered HPV DNA tests in addition to pap smear tests.
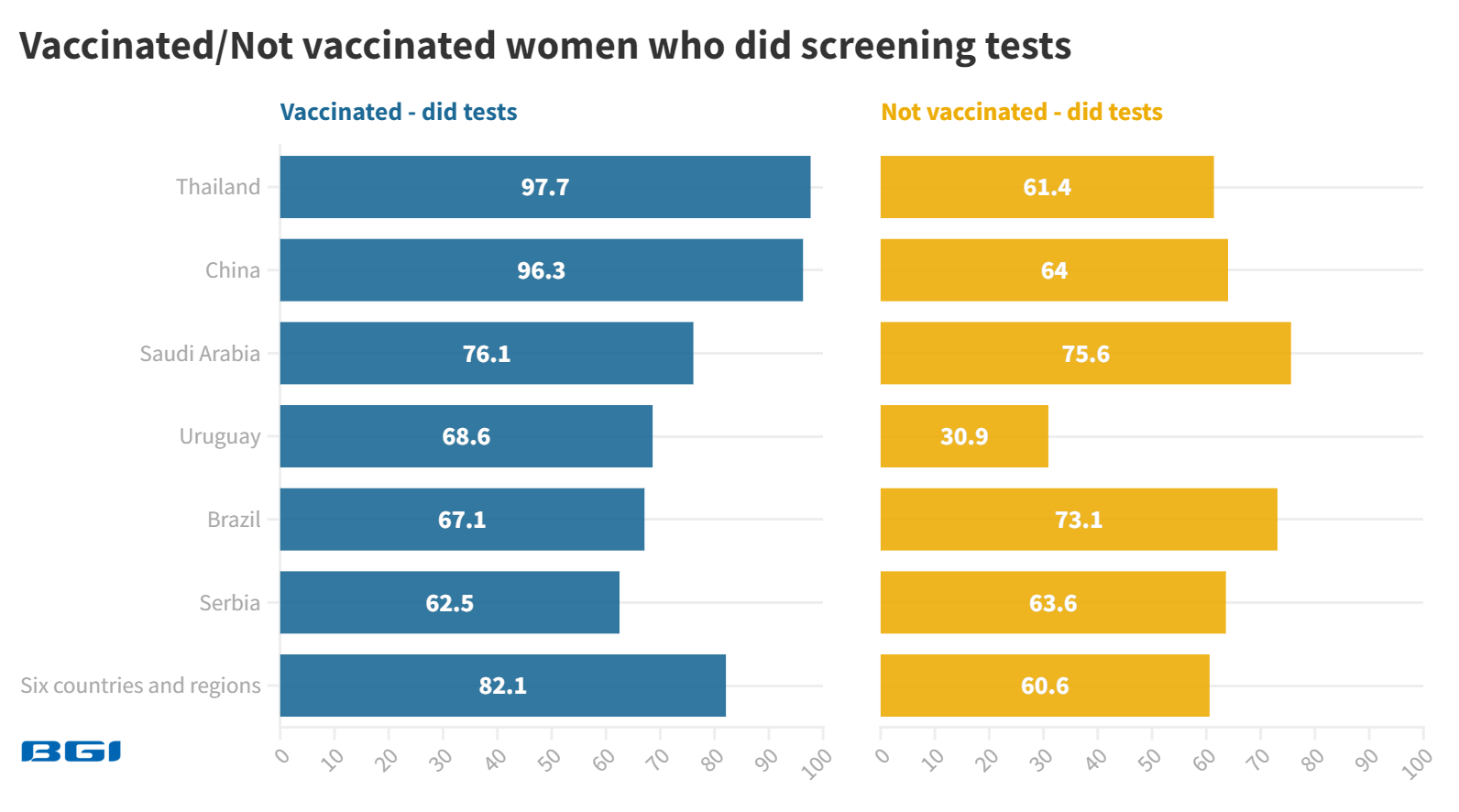
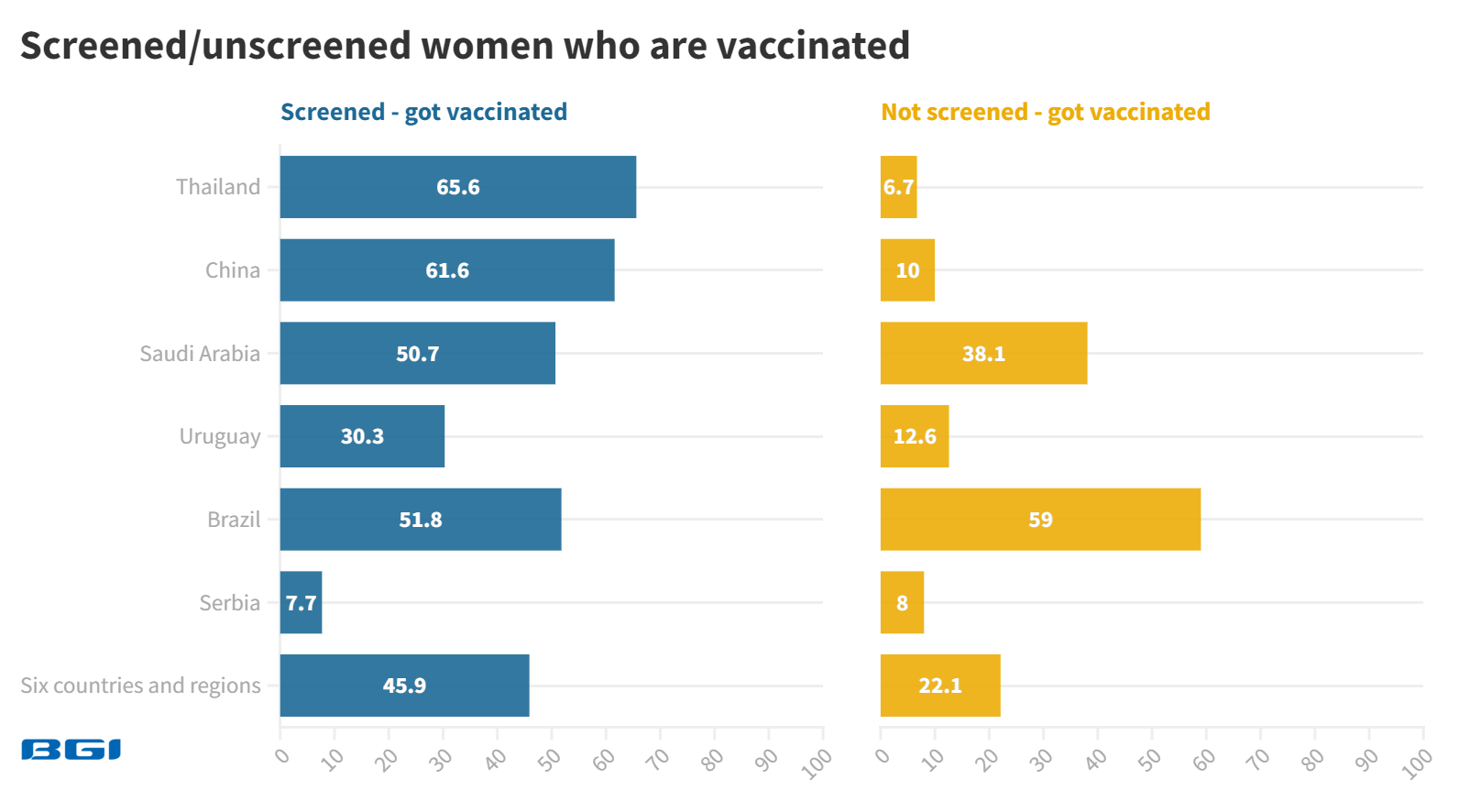
Vaccination and screening form a virtuous cycle: For women who had the HPV vaccine, 82.1% had a cervical cancer screening, significantly higher than 60.6% of unvaccinated women. For women who had undergone screening, 45.8% received the HPV vaccine, which is higher relative to 22.1% of unscreened women.
Informing women who missed national vaccination programs about where and when they could get vaccinated and screened is vital. Zhang Lin, BGI Genomics Senior Product Manager, notes, "Early cervical cancer detection is vital to save lives and eventually eliminate this dreaded disease in line with WHO's global strategy. This study shows increased awareness of women could be the missing link to boost vaccination and screening rates further."
Cervical Cancer Screening Awareness
Cervical cancer can be cured if diagnosed early and treated promptly. The WHO recommends screening starting from 30 years of age in the general population of women, with regular HPV screening every 5 to 10 years. As women living with HIV are six times more likely to develop cervical cancer, they should be screened more frequently, every 3 to 5 years.
Source: UN Twitter account
Is there a screening awareness gap?
40.0% worldwide did not know that over 95 percent of cervical cancer is caused by HPV. Saudi Arabia (51.2%) and Thailand (47.3%) are the most unaware of this fact.
31.2% worldwide never had a cervical cancer screening. Among women who are unaware cervical cancer is often caused by HPV, 39.1% of them never had a cervical cancer screening which is higher than the global average. Saudi Arabia (55.8%) and Serbia (36.5%) have the highest percentage who never had a cervical cancer screening. Therefore, there appears to be an awareness gap that impacts cervical cancer screening rates.
What do women know about cervical cancer screening?
Twice as many women worldwide heard of pap smear (81.0%) versus HPV DNA test (38.9%). Serbia (95.1%) and Brazil (91.1%) are the most aware of pap smears, while the Chinese mainland (64.8%) and Thailand (50.5%) lead in terms of HPV DNA test awareness.
88.0% worldwide are more likely to choose the HPV DNA test (95% accuracy rate) over a pap smear (80-90%) upon learning about its higher accuracy. Thailand (94.0%) and the Chinese mainland (92.3%) had the highest percentage of those choosing the HPV DNA test over a pap smear.
77.9% worldwide are aware HPV is a sexually transmitted virus. Saudi Arabia (55.3%) and the Chinese mainland (72.9%) have the lowest percentage who know HPV is a sexually transmitted virus.
What's holding women back from cervical cancer screening?
The absence of symptoms (42.3%), fear of results (40.7%), and embarrassment of meeting a male doctor performing a pap smear (39.0%) are the top reasons stopping women from cervical cancer screening. The absence of symptoms is top in Uruguay (55.9%) and Brazil (51.1%), while fear of results is highest in the Chinese mainland (59.4%) and Saudi Arabia (44.9%).
57.1% in the Chinese mainland and 51.9% in Saudi Arabia indicate the embarrassment of meeting a male doctor performing a pap smear is holding them back from screening tests. Among the women from 21-25 years old, 43.5% (highest among the age groups surveyed) are deterred by meeting a male doctor performing a pap smear.
Doctor's recommendation (75.9%) is the top reason pushing women toward cervical cancer screening. Behavior-based factors such as new sexual partners or finding out their sexual partner is not monogamous (25.5%) rank much lower. Doctors may ask women about their symptoms and behavior-based factors to make informed recommendations.
Cervical Cancer Vaccination Awareness
The WHO notes a deeply concerning decline in HPV vaccination coverage globally during COVID-19. Between 2019 and 2021, coverage of the first dose of HPV vaccination fell by 25% to 15%. 3.5 million more girls missed HPV vaccination in 2021 compared to 2019. Countries must step up their HPV vaccination programs to reverse the declines in coverage.
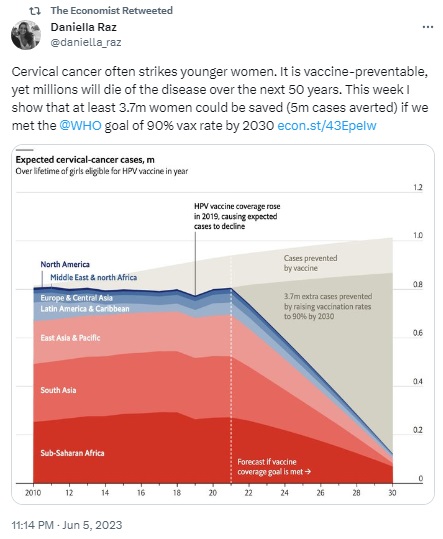
Source: The Economist Twitter account
Is there a vaccination awareness gap?
Not knowing where to get vaccinated (38.7%) is the top reason stopping women from cervical cancer vaccination, followed by the absence of symptoms (36.8%) and fear of side effects (28.6%). Thailand (50.8%) and Serbia (49.5%) have the highest percentage who do not know where to get vaccinated.
38.4% worldwide received the HPV vaccine. Serbia (7.8%) and Saudi Arabia (29.5%) have the lowest percentage who received the HPV vaccine. Meanwhile, for those aged 21-25 years old, 46.0% of them received this vaccine which is higher than the global average.
What do women know about cervical cancer vaccination?
HPV vaccines work best if administered before exposure to HPV and sexual activity. Therefore, to provide better protection against cervical cancer, in its position paper published in Dec 2022, the WHO recommends vaccinating girls aged 9 to 14 years and the following vaccination schedule:
- A one or two-dose schedule for girls aged 9-14 years
- A one or two-dose schedule for girls and women aged 15-20 years
- Two doses with a 6-month interval for women older than 21 years
43.2% worldwide are aware about the WHO-recommended age range (9 to 14 years) to begin vaccination. Saudi Arabia (20.8%) and Thailand (25.4%) have the lowest percentage who are aware of this WHO-recommended age range.
Only 17.9% worldwide know the vaccination schedule across various age groups, e.g. two doses with a 6-month interval for women older than 21 years. Brazil (10.2%) and Serbia (14.0%) have the lowest percentage who know the relevant vaccination schedule.
The Relationship between Cervical Cancer Screening and Vaccination Awareness
The WHO notes a coordinated cervical cancer prevention strategy should include education about reducing behaviors that increase the risk of acquiring HPV infection and information about screening, vaccination, diagnosis, and treatment of precancerous lesions, cancer, and risk factors.
HPV vaccination is a primary prevention intervention and does not eliminate the need for screening later in life since the existing vaccines do not protect against all high-risk HPV types and will have a limited impact on disease in unvaccinated women and those vaccinated at older ages.
Source: American Association for Cancer Research (AACR) Twitter account
Are there synergies between screening and awareness?
Of those who had the HPV vaccine, 82.1% also did cervical cancer screening, significantly higher than the unvaccinated average of 60.6%. In Thailand, 97.7% of vaccinated women had a test, much higher relative to 61.4% of unvaccinated women.
Not all were vaccinated before screening tests, so this study also examined whether those who went for screening tests were more likely to be vaccinated. 45.9% of these women received the HPV vaccine, which is higher relative to 22.1% of unscreened women.
About BGI Genomics and SENTIS HPV Tests
BGI Genomics, headquartered in Shenzhen, China, is the world's leading integrated solutions provider of precision medicine. In July 2017, as a subsidiary of BGI Group, BGI Genomics (300676.SZ) was officially listed on the Shenzhen Stock Exchange.
The CE-certified SENTIS™ HPV test combines self-sampling technology and genotyping assay to detect 14 most important, "high-risk" types of HPV, including HPV -16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68 and 2 "low-risk" types of the virus, HPV -6, 11. HPV genotyping detection is based on Next Generation Sequencing (NGS) technology based on a large sample volume for each run, which decreases the testing cost for each individual. In 2021, the WHO recommends DNA testing as a first-choice screening method for cervical cancer prevention.
Methodology
This study is based on an online survey of 1,878 female respondents from Brazil (315), the Chinese mainland (310), Saudi Arabia (312), Serbia (307), Thailand (319), and Uruguay (315).
These respondents were based in their respective country or region when this survey was conducted in July 2023. Surveys were conducted in local languages. Respondents were aged between 21 to 45 years old. Momentive Global was commissioned to carry out this survey.
Read More: